Unfortunately, there is still very little coverage to pay for weight loss medications around the world. In most countries, people who want weight loss medications have to pay out of their own pocket. There are a few countries who pay for weight loss medication, though who can get them covered, and for how long, is often restricted (the UK as an example, blogged previously here). In Canada, about a third of private medical plans pay for weight management medication, and there is no public coverage.
So how do we change this? How do we get payors to cover weight management medication?
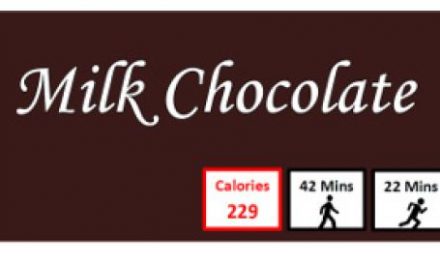
The next step forward, in my view, is to prove the benefit of weight loss medication to treat specific health issues associated with elevated weight, hopefully leading to insurance and/or public coverage of medication for that specific health condition. Payors assess cost effectiveness of any medication, and if money can be saved in treating obesity-related health conditions by using weight management medication, then payors may be more likely to cover that medication.
We already have data to support obesity medication to improve some obesity-related health issues. In our recent Canadian Obesity Guidelines Pharmacotherapy (medication) chapter update (in which I’m the lead author), based on these data, we generated two new recommendations, for obesity medication showing benefit of weight management medication in people with obesity and fatty liver disease, and obstructive sleep apnea. (We already had recommendations for obesity medication in people with type 2 diabetes and prediabetes, and we expanded on these as well.)
Fortunately, studies of weight management medications are currently underway in people with obesity-related health concerns such as cardiovascular disease, heart failure, osteoarthritis, fatty liver disease, and more. Some of these studies will provide longer term data as well, addressing the concern that some payors have raised about paying for treatment long term, including the UK.
Will obesity medication ever be covered for people who don’t yet have any health issues associated with elevated weight? While some may argue that as a person with elevated weight and no health complications doesn’t have ‘obesity’, we also know that healthy people with elevated weight are at high risk of developing health complications down the road. Thus, treating elevated weight (and access to treatment) is important not only for people with health complications, but also those who don’t yet have health complications.
There remains also a pervasive stigma and bias against people with obesity amongst insurers, the public, and the health care system in general. Insurers that do not cover obesity treatment list obesity as a ‘lifestyle issue’, when it is well accepted globally that obesity is a chronic medical condition that requires attention, care and treatment. So, we still have a long way to go in breaking down obesity bias and educating insurers about the importance of covering obesity treatments.
Payors surely have concerns about inappropriate use of obesity medication as we have seen pervading social media outlets and media in the last months. I fully agree that this is a concern, and that physicians must prescribe obesity medication appropriately.
While we sure hope coverage of weight management for any person in whom use of these medications is appropriate will become a reality, the cost of public programs paying for weight loss medications for everyone who could benefit is probably not realistic, unless the cost of obesity medication drops substantially (listen to a New England Journal of Medicine podcast on the US perspective on this here). The more evidence we generate for obesity medications to treat weight-related health conditions, the closer I hope we will come to broader coverage opportunities.
Share this blog post using your favorite social media link below!
Check me out on twitter! @drsuepedersen
www.drsue.ca © 2023