This weekend, I’ve had the pleasure of attending and being invited to speak at the inaugural meeting of the Canadian Association of Bariatric Physicians and Surgeons in Toronto. While I will share with you the information from my talk in an upcoming post (which was about the treatment of diabetes with obesity surgery), what I would like to share with you today is a fantastic debate held this morning, about which type of obesity surgery is the ‘best’ overall surgery.
The three main types of bariatric (obesity) surgery were compared:
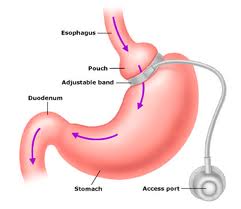
1. Gastric Banding: This is an inflatable band that is placed around the upper part of the stomach. It works by making the reservoir of the stomach smaller, so that only small amounts of solid food can be consumed, resulting in a sense of fullness after only a small amount of food. The band can be adjusted to make it looser or tighter by filling or deflating it with salt water via a port that lies just under the skin.
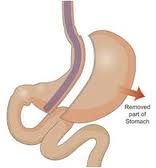
2. Sleeve Gastrectomy: In this surgery, most of the stomach is removed, and the shape of the remaining stomach looks like a ‘sleeve’ – hence the name.
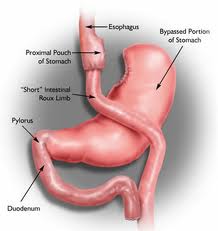
3. Gastric Bypass: This surgery is the most complex of the three. First, the stomach is made smaller (though the rest of the stomach is not physically removed). Next, the small intestine is rerouted so that food bypasses the first part of the intestine, and absorption of nutrients first begins about 1.5 meters further down the intestinal canal.
Dr David Urbach of the University of Toronto began the debate with a discussion of the laparascopic adjustable gastric band. On the positive side, the early complication rate of gastric bands is lower than for sleeve gastrectomy or gastric bypass. However, the gastric band is not as effective to produce weight loss, and it’s not as good to improve complications of obesity (eg diabetes, high blood pressure, sleep apnea). Over the long term, gastric banding is not looking very good – as blogged previously, at 12 years after gastric banding, one study showed that 60% of people who had gastric banding needed a reoperation of some kind. At 10 years, about half of patients have had their band removed (either because of complications, or because it was not effective). While some people do have sustained weight loss over the long term with a band, a substantial proportion regain weight as well.
Dr Urbach concluded that gastric banding is probably not a good long term treatment for obesity, nor for the medical problems that go along with obesity. He went so far as to say that the band is perhaps best considered only as a cosmetic procedure for patients wishing for weight loss.
Dr James Ellesmere of Dalhousie University reviewed sleeve gastrectomy. He started off by noting that the sleeve is also quite a safe procedure to perform, with a low complication rate and a low risk of needing reoperation in the future. In terms of short term risk of surgery, the risk is a bit higher than the short term risk of gastric banding, but lower than the risk of gastric bypass surgery. The success in weight loss falls between banding and gastric bypass, and the improvement in complications of obesity (diabetes, sleep apnea, high blood pressure etc) also falls between banding and bypass. An important down side of sleeves is that it is a newer procedure, and therefore, not much is known about long term efficacy (very few studies over 5 years exist). The few studies that do exist show that there is variability in long term results – as with all of these surgeries, weight regain can occur.
Bottom line of sleeve gastrectomy: It falls between gastric bands and gastric bypass in terms of benefits and risks, and we don’t yet have a lot of long term data (though this data is coming).
In regards to gastric bypass surgery, Dr John Hagen of the University of Toronto reviewed data that show that gastric bypass is the most effective of these surgeries to cause weight loss, and to improve diseases associated with obesity (diabetes, sleep apnea, etc). As such, it is considered the gold standard surgery in many centres. However, there is a significant downside as well: as it’s the most invasive surgery, there is higher short term operative risk. In addition, because food is not digested in the first part of the intestine, many crucial nutrients are not sufficiently absorbed from a regular diet – therefore, the patient undergoing this surgery must be prepared to take a mandatory array of vitamins and nutrients for the rest of their lives.
Bottom line: Gastric bypass has the highest success rate, but also the highest risk.
My take on this discussion? As always, the decision to undergo obesity surgery is a very serious one, and every person is different. Risks and benefits not only of the types of surgery, but of surgery in general, must be carefully weighed by the patient and their health care providers. In terms of which type of surgery to choose, gastric banding does not appear to be a good long term treatment strategy; gastric bypass surgery and sleeve gastrectomy appear to be the best options to consider.
Dr Sue Pedersen www.drsue.ca © 2012 drsuetalks@gmail.com
Follow me on Twitter for daily tips! @drsuepedersen