NEW ON DRSUE.CA! Prefer to listen? Check out my audio recording of this post here:
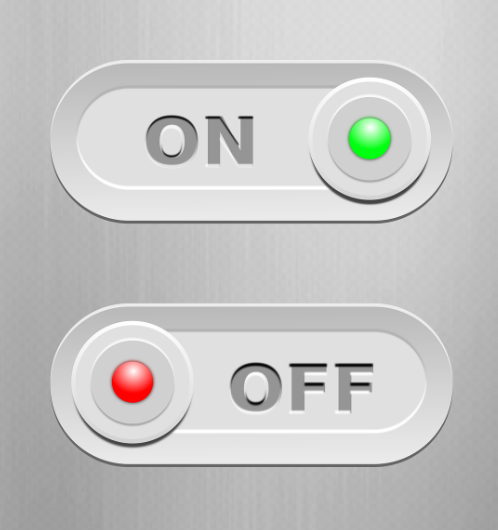
The science behind weight regulation leaves no doubt that for the vast majority of people with obesity, weight management needs to be long term. However, given that weight management medication is expensive, and given that many people may prefer not to be on medication long term, the question continues to arise (from patients, payors, and health care providers alike) as to whether intermittent on/off treatment may be something we need to seriously consider.
While there are no clinical trials looking at intermittent treatment, let’s first review what we know about what happens when weight management is stopped.
Every study of weight management medication shows that when medication is stopped, weight starts to go back up, even in the first month off of treatment. This is because the medication provides a defense against our natural human biology which powerfully drives weight regain after weight loss. When medication is stopped, that defense is gone, hunger returns or increases with a vengeance, and weight almost always goes back up. We can draw similar analogies from other chronic medical issues like hypertension: if you have good blood pressure control with medication, then stop the medication, what happens? Blood pressure goes back up. The blood pressure medication was controlling high blood pressure, not curing it. Same goes for obesity medication.
More recently, we have a couple of studies looking at weight after a full year off of weight management medication.
In the STEP 1 study of semaglutide 2.4mg (Wegovy, also known as Ozempic at lower doses for type 2 diabetes) vs placebo, patients lost a mean of -17.3% with semaglutide 2.4mg vs -2% with placebo. In the STEP 1 extension study, patients were followed for a year after stopping treatment. After a year off of semaglutide, the group had regained an average of 11.6% weight – in other words, they were still down -5.6% in weight compared to before starting semaglutide. However, it is important to point out that the trajectory of the weight regain was still going up. If people had been followed further than 1 year, it is therefore likely that weight regain would have continued.
In the SURMOUNT 4 study of tirzepatide (Zepbound) (also known as Mounjaro for type 2 diabetes), the results of which have been presented but not yet published, all patients in the study received tirzepatide for the first 36 weeks. At 36 weeks, the mean weight loss was -20.9%. For the next year, half of patients were randomized to continue tirzepatide at the maximally tolerated dose (10mg or 15mg weekly), and half stopped. Those who continued tirzepatide lost additional weight, for a total weight loss of -25.8%. Those that stopped medication regained just over half of the weight they had originally lost, though their weight was overall still -9.5% lower than their weight at the start of the study. Again here, the trajectory of the weight regain curve was still going up at the end of the study, suggesting that if the study had been continued for longer, that weight regain would have been seen to continue.
So, with an on/off (intermittent) treatment approach, I would be concerned that weight will yo-yo up and down, and we know that this is damaging to our metabolism, making future weight loss attempts even harder (as blogged previously here and here). We must also remember that when we are treating with weight management medication, we are improving/treating many other medical issues concomintantly, such as blood sugars, blood pressure, fatty liver disease, sleep apnea, heart failure, and so on. With an on/off treatment approach, I would be very concerned that these other weight-related health issues would deteriorate along with the weight regain phase of each yo-yo cycle. With semaglutide 2.4mg now being proven to reduce cardiovascular events in people with obesity and cardiovascular disease, I would also be concerned that having only intermittent effect of semaglutide may not be enough to reduce heart attack and stroke risk. To draw an analogy, we would not suggest intermittent treatment of cholesterol for these people – we want long term continued treatment to provide long term benefit.
In the context of current shortages of semaglutide and tirzepatide, some people have been forced into an intermittent treatment regimen, and the global clinical experience has been that of regain in weight, deterioration in other health parameters, and distress to the individual struggling physically, mentally, and from a quality of life perspective during the time that they can’t get their medication. I personally do not feel that we need clinical trials of intermittent therapy to tell us that this approach will not be of benefit.
In the name of cutting cost of these expensive meds, could a lower maintenance dose be effective to control weight and related health issues long term? I think it would be reasonable to do studies to answer this question. That being said, in my experience with my own patients, when they decide they really want to try reducing the dose, the overwhelming majority end up experiencing weight regain, and end up deciding to go back to the full dose that they were taking to begin with.
At some point, the patents will expire on these medications, allowing biosimilar (‘generic’) versions to be produced and purchased at a lower price. Liraglutide (trade name Saxenda for obesity, Victoza for diabetes) will be the first to lose its patent, with biosimilar versions starting to emerge next year. Until these medications are more reasonable in cost, and until the supply of these medications can meet the ever increasing demand, there may be no choice but to find alternative strategies. Treating at a lower dose consistently, in my view, would be better than an on/off approach.
Disclaimer: I am/have been an investigator in clinical trials of semaglutide, tirzepatide, and liraglutide. I receive honoraria as a continuing medical education speaker and consultant from the makers of semaglutide and liraglutide (Novo Nordisk) and Eli Lilly (tirzepatide).
Follow me on X (twitter): @drsuepedersen
Share this blog post using your favorite social media link below!
www.drsue.ca © 2023