At this week’s World Diabetes Congress in Dubai, hosted by the International Diabetes Federation, I had the opportunity to listen to a fantastic debate as to whether bariatric (weight loss) surgery is an appropriate treatment option for Type 2 Diabetes.
The argument in favor of bariatric surgery was presented by Dr Francesco Rubino, a bariatric surgeon and leading authority on the issue from Cornell University, in New York. He highlighted key points of evidence regarding the benefits of bariatric surgery in terms of improving diabetes, noting that bariatric surgery provides a powerful potential opportunity to reverse the course of an otherwise progressive disease. While the current criteria for bariatric surgery in diabetics include a Body Mass Index (BMI) ≥35, he presented for us the International Diabetes Federation position statement on the role of bariatric surgery, which suggests that surgery should also be considered in people with BMI 30 to 35 when diabetes cannot be adequately controlled by medical therapy, especially in the presence of other cardiovascular risk factors. (BMI can be calculated here)
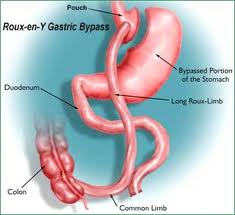
Dr Rubino noted that bariatric surgery stands apart from some other medical treatments of diabetes, in that many medications cause weight gain, whereas bariatric surgery can result in substantial weight loss. He noted that patients who are most likely to have the greatest improvement (or complete remission) of diabetes include those with a shorter duration of diabetes, and lower preoperative medication requirements; in other words, earlier intervention appears to produce the best results. He noted that not only does bariatric surgery improve diabetes, but can also be very effective to prevent new cases of diabetes. Other benefits include some improvement in cholesterol profile and blood pressure, which are also risk factors for cardiovascular disease. Gastric bypass is superior to gastric banding in achieving these effects. (Sleeve gastrectomy was not discussed in particular – I enter my own editorial comment here, that sleeves are proving to be quite effective to treat type 2 diabetes as well, somewhere between gastric bypass and banding in terms of efficacy, but so far appearing to be closer in efficacy to gastric bypass).
In discussion of the very limited accessibility to bariatric surgery, Dr Rubino provocatively noted:
“If there were a pill or a shot that can control blood sugars, improve body weight, cholesterol and blood pressure, and improve survival, would it be acceptable that >99% of people do not have access to the treatment? ”
He concluded with the comment that we should not be using BMI as the most important criteria or cutoff in choosing the right patient for bariatric surgery; rather, we should be considering the metabolic disease (in particular, diabetes) that each patient carries, and stratify our decision re surgical candidates based on cardiovascular risk profile, as the BMI does not tell the whole story.
The negatives for bariatric surgery in the treatment of type 2 diabetes was presented by Dr John Pinkney, professor of diabetic medicine from Plymouth, UK.
Dr Pinkney opened with a discussion of the treatment goals for type 2 diabetes, including increasing life expectancy, reducing cardiovascular disease, reducing small vessel complications of diabetes (eye, kidney, and peripheral nerve complications), and improving quality of life, using treatment modalities where the benefits exceed the risks. Many of these health goals are achieved by optimizing control of vascular risk factors (diabetes control, blood pressure, and cholesterol).
In terms of treatment targets for diabetes, Dr Pinkney notes that several recent diabetes trials have suggested that tight glucose control may not actually prevent cardiovascular events, compared to slightly less tight glycemic control. He wondered, then, whether getting diabetes into excellent control with bariatric surgery would really be of that much benefit (and worth the risk?) in patients who had reasonable control of their diabetes in the first place.
He noted that while the improvements in blood pressure and cholesterol with bariatric surgery are statistically significant, that the absolute improvements are not that big. From the prevention of small vessel diabetes complications perspective, he noted that there is not yet much study in this area, and the question as to whether bariatric surgery prevents these diabetes complications in the long term remains unanswered.
While improvements or remission of diabetes is certainly impressive, the long term durability of diabetes remission was discussed, in that the most recent literature is now suggesting that a substantial proportion of diabetes that initially goes into remission, recurs years down the road.
The downsides of bariatric surgery require very serious consideration, and the risks vs benefits must be weighed carefully. The risk of death due to the surgery itself was discussed, though Dr Rubino noted that this risk is approximately that of a gall bladder removal surgery (ie, fairly low as far as surgeries are concerned). Although the need for diabetes medications may decrease with surgery, these treatments are ‘traded in’ for the need for a new array of lifelong nutritional supplements (the exact array of supplements needed depends on the type of surgery). Not taking these supplements or not having them monitored carefully can result in life threatening complications. The removal of the freedom to ‘eat as I wish’ and the potential impact on quality of life was also noted.
Dr Pinkney noted that type 2 diabetes is a complex disease that is very common, and suggested that it may not be feasible or productive in general to consider a treatment (surgery) that is very expensive, requires lifelong follow up, and is therefore not accessible for any but a small sliver of the people with diabetes worldwide.
Both presenters were grateful for the opportunity to present this important topic, noting that the topic of bariatric surgery has only been taken seriously as a potential therapy for diabetes in the last few years.
At the conclusion of the presentations, a show of hands of the audience was requested as to how many people were in favor vs against the use of bariatric surgery to treat type 2 diabetes (this was an auditorium containing several hundred diabetes health care professionals from around the world) – to my eye, the vote was roughly evenly split.
My feeling on this issue is reflected in an underlying theme to both of these presentations: the decision for bariatric surgery is a highly patient specific decision. Each patient must be considered on a case by case basis, with the benefits and risks carefully weighed and discussed in exquisite detail. For the right diabetic patient, bariatric surgery can provide an appropriate treatment option.