In follow up to my recent blog post – as promised – the hotly anticipated LEADER trial results became available this week, in a simultaneous release at the American Diabetes Association meeting, as well as published in the New England Journal of Medicine.
The LEADER trial examined the effect of a type 2 diabetes medication called liraglutide (trade name Victoza) on cardiovascular events, in a group of people with type 2 diabetes who were deemed to be at high cardiovascular risk (age 50 or more with at least one existing cardiovascular condition such as a history of heart attack or stroke; or age 60 or more with at least one cardiovascular risk factor (for example, hypertension).
The goal of this study, as for all hard outcome studies of diabetes medications, was to prove cardiovascular safety of liraglutide.
Not only did liraglutide prove to be safe in people at high cardiovascular risk – it actually REDUCED cardiovascular events. Amongst 9,340 patients from 32 countries, followed for a median of 3.8 years, there was a 13% reduction in the risk of (a composite endpoint of) death from a cardiovascular causes, non fatal heart attack, and non fatal stroke. Cardiovascular deaths were reduced by
22%, and death from any cause was reduced by15% compared to placebo. The benefit of liraglutide was particularly pronounced in people who had established cardiovascular disease at baseline, and in those with moderate reduction in kidney function at baseline.
To put the results another way:
- 66 people would need to be treated for 3 years to prevent one of (cardiovascular death or heart attack or stroke)
- 98 people would need to be treated for 3 years to prevent one death of any cause.
These numbers needed to treat are similar to the protective effects of statins (cholesterol medications) and ACE inhibitors (blood pressure medication).
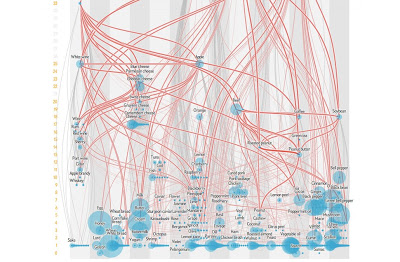
Now that we know that liraglutide has a distinct cardiovascular benefit, a question that arises is whether this is an effect shared by other medications in this class, called GLP-1 receptor agonists. The ELIXA trial, a study of lixisenatide (not available in Canada), did not show a cardiovascular benefit. Studies of other medications in this class (eg dulaglutide, exenatide) are still underway, so for these, we don’t know the answer yet.
We also don’t know if the cardiovascular benefit of liraglutide exists in people with type 2 diabetes who aren’t in these high risk groups, or in people with obesity without type 2 diabetes (liraglutide is also available as an obesity treatment, called Saxenda). However, this trial gives us additional confidence in the safety of liraglutide, given that the LEADER trial was conducted in the highest cardiovascular risk population.
The effect of liraglutide to reduce cardiovascular events is important, as we know that cardiovascular disease is the leading cause of death in people with type 2 diabetes. So far, other diabetes medications that have shown a cardiovascular benefit are metformin (with somewhat scanty data) and empagliflozin (based on the EMPA-REG trial, which you can read about here). Thus, in Canada, metformin is considered the first line treatment for type 2 diabetes, with empagliflozin to be considered in patients with existing cardiovascular disease who are not at target blood sugar control with metformin.
Liraglutide will likely join the ranks of empagliflozin as a second line treatment option, with the decision making process as to which to choose based not only on the characteristics of each medication, but most importantly, on the characteristics and desires of each individual patient.
Follow me on twitter! @drsuepedersen
Disclaimer: I have been involved in research trials of liraglutide, other GLP-1 receptor agonists, and SGLT2 inhibitors like empagliflozin. I receive honoraria as a continuing medical education speaker and consultant from the makers of liraglutide (Novo Nordisk) and empagliflozin (Boehringer-Ingelheim/Eli Lilly).