We know that there is a relationship between mental health and obesity, with mental health issues such as depression being associated with an increased risk of obesity, and with
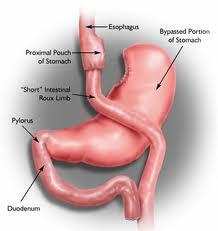
the risk of mental health issues developing increasing as weight increases. In people with more pronounced obesity who are considering bariatric surgery as a treatment option, it is important to consider how mental illness may impact theefficacy and safety of surgical treatment for obesity.
These issues were beautifully summarized in a recent review by Val Taylor and colleagues, published in the Canadian Journal of Diabetes, with a focus on Canadian data.
Here are a few of the highlights:
1. How common are mental health issues in Canadian bariatric surgery patients? Over half of patients presenting in Ontario for bariatric surgery had a history of mental illness (most commonly depression). Neither a history of depression nor bipolar disorder seem to be associated with success of weight loss with bariatric surgery, but stability and control of mental health issues preoperatively is important to optimize success.
The prevalence and severity of depression in the bariatric population are consistently decreased after surgery – but there is a risk of development of depression for some people as well, which may be related to some of the
psychological challenges that can present after surgery.
Many people with mental health issues are taking medications to treat these conditions, and absorption of these meds may
be affected after surgery, so close monitoring to ensure good control of the mental health issue after surgery is important.
2. Eating disorders:
Binge eating disorder (BED) has a prevalence of up to 30% in people presenting for bariatric surgery, with the data conflicting on whether BED reduces the success of weight loss with bariatric surgery. Management of the feeling of loss of control and regulation of emotions in these individuals are important factors to help reducing binge eating in this group.
Active bulimia is a contraindication to bariatric surgery.
3. Suicide risk:
While depression usually improves after surgery, the risk of suicide is increased after bariatric surgery, with a multitude of possible reasons/contributors behind this fact. The risk of self harm seems to be increased at least 3 years after surgery, so long term psychological follow up and support of bariatric patients is essential.
4. What if there is a past history of sexual abuse?
A history of sexual abuse is present in 21.5% of people in the Ontario Bariatric Surgery Registry. While this does not appear to influence the success of surgery, these individuals are at a higher risk of mental health issues such as depression, speaking to the need for proper assessment and follow up.
5. Substance use/abuse:
A history of substance use (alcohol, tobacco, or recreational/illicit drugs) seems to be correlated with a risk of substance use after surgery, particularly if the substance use
history is near to the time of surgery. Alcohol abuse is a particular risk, as alcohol hits harder and fasterafter surgery. A ‘transfer’ of addictions from one thing to another (eg, from food to gambling) after surgery has been described, and should be discussed and managed ahead of time.Most often, mental health issues can generally be well managed to optimize success of the individual undergoing bariatric surgery. Identifying and managing these issues before surgery is essential, and long term support after surgery is key as well.