When I meet a patient with diabetes who uses insulin, it is not uncommon for them to ask me whether they have type 2 or type 1 diabetes. Other doctors sometimes refer their patients to me specifically to determine if that person has type 2 or type 1 diabetes.
So: What’s the difference between type 2 and type 1 diabetes – and why does it matter?
Type 2 diabetes is the most common type of diabetes. The underlying problem in type 2 diabetes is that the body is resistant to the effects of insulin. This means that the pancreas has to work in overdrive to make enough insulin to keep blood sugars normal. After years of working in overdrive, the pancreas gets tired, and is no longer able to make enough insulin to keep blood sugars normal. Blood sugars then start to climb into the prediabetes range, and ultimately into the diabetes range.
Type 2 diabetes has a strong genetic predisposition, often (but not always) with a strong family history of diabetes. About 90% of people with type 2 diabetes have overweight or obesity. Insulin resistance gets worse with weight gain and better with weight loss, so type 2 diabetes can improve with weight loss in people who carry excess weight.
Type 2 diabetes is most commonly diagnosed in adulthood, but the age at which we are seeing new type 2 diabetes gets younger and younger, in concert with the rise of obesity (which is a risk factor for developing type 2 diabetes). Type 2 diabetes is becoming more and more common in children, even as young as preschoolers.
Type 1 diabetes happens when the immune system attacks the cells in the pancreas that make insulin, and is therefore what we call an autoimmune disease. There is a genetic susceptibility to type 1 diabetes, but most often there is no family history of diabetes (though there is often a family history of other autoimmune conditions). We are not sure exactly what triggers type 1 diabetes, but many possibilities have been considered, including viruses or other environmental factors.
Type 1 diabetes is most commonly diagnosed in childhood or early adulthood, but it can come on in later adult years as well. A few times each year, I diagnose a person in their 50s or 60s with type 1 diabetes (though this is rare).
For more on type 2 vs type 1 diabetes, as well as other rare forms of diabetes, check out the Diabetes Canada chapter on this topic.
Why does it matter if you have type 2 or type 1 diabetes?
The biggest reason why this distinction is important is because it affects what treatment options are appropriate for you.
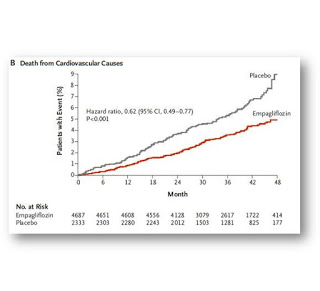
There are 9 classes of medications for type 2 diabetes. We usually start with metformin, which works by decreasing the body’s resistance to insulin. From there, the choices are usually geared towards avoiding medications that cause weight gain (as most people with type 2 diabetes also struggle with weight), avoiding risk of low blood sugars, taking the stress off the pancreas, and most importantly, providing cardiovascular and kidney protection. As the pancreas is genetically programmed to get more tired with time, and also because it is constantly working in overdrive, many people with type 2 diabetes go on to require insulin. As an endocrinologist, most of the type 2 diabetes patients I see have had diabetes for many years, so many of them need insulin as part of their treatment.
In type 1 diabetes, the pancreas stops making insulin. Insulin is a hormone that is essential for life. So, the treatment of type 1 diabetes is insulin. However, people with type 1 diabetes who also struggle with overweight or obesity may benefit from adding in some medication options that are intended for people with type 2 diabetes (note that these medications are ‘off label’ in type 1 diabetes).
Share this blog post using your favorite social media link below!
Follow me on twitter! @drsuepedersen
www.drsue.ca © 2021