Gastroparesis is a condition where there is delayed emptying of the stomach due to slowed muscle function of the gastrointestinal tract (ie without an actual physical blockage). Symptoms can include nausea, vomiting, a feeling of fullness/bloating soon after eating, belching, and/or stomach pain. A gastric emptying study (food with a radioactive label is consumed and measurements are taken of how much is left in the stomach after 4 hours) is required to make the diagnosis of gastroparesis, along with an upper endoscopy (camera into the stomach) to rule out a mechanical (physical) obstruction. Retention of >10% of food in the stomach after 4 hours on the gastric emptying study reflects delayed gastric emptying.
Can GLP1 receptor agonists cause gastroparesis?
We know that GLP1 receptor agonists (GLP1RAs) slow down gastrointestinal (GI) transit. This is the reason why some people get side effects like nausea/vomiting, constipation, diarrhea, and/or heartburn. If these side effects occur, they are usually mild to moderate, temporary in nature, and mostly seen during the dose escalation phase. Once on a stable dose, this effect abates for most people. If GI side effects are experienced, they can often be lessened with slower dose escalation, or backing off on the dose and then retitrating more slowly. Some people have a maximum dose of GLP1RA that they tolerate, as they have GI symptoms on higher doses. A small proportion of people do not tolerate any dose of GLP1RA due to GI side effects.
We would not typically do testing for gastroparesis (which, remember, requires the radioactive label study to diagnose) when people have GI side effects – rather, we would take steps above to alleviate symptoms of slowed gastointestinal transit. (Note also that avoiding high fat and spicy food during dose escalation, focusing on eating smaller portions, and mindfulness of the satiety sensation that GLP1RA provides can also help avoid these symptoms.) Testing for gastroparesis has not been done in clinical trials, as we allow the symptoms to guide us in how much medication a person can tolerate, or whether we need to back off on the dose or stop medication entirely. (Note: For liraglutide (Victoza/Saxenda) and semaglutide (Ozempic/Wegovy), studies suggest that the GI slowing effects are mostly temporary in nature, but may be more persistent for the shorter acting twice daily exenatide (Byetta). In my clinical experience, for some people, the GI side effects with any of these medications are not temporary and do not go away until the dose is decreased or stopped.)
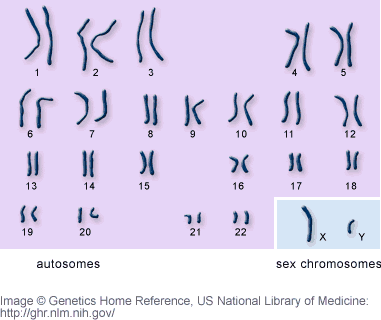
Some people with diabetes have gastroparesis, which is a known potential neurological complication of diabetes (a form of autonomic neuropathy). GLP1RAs are widely used in people with type 2 diabetes. There is limited information on the effect of GLP1RAs in people with pre-existing gastroparesis. People with known gastroparesis are often not included in clinical trials of GLP1RAs because of the concern that gastroparesis could worsen. One very small study in people with gastroparesis showed no additional delay of gastric emptying 3 days after starting exenatide (a GLP1RA) compared to pre-treatment. Some experts recommend avoiding GLP1RAs altogether in people with pre-existing gastroparesis, due to concern that it could worsen symptoms. GLP1RAs could perhaps also bring on symptoms in a person who had non-symptomatic milder autonomic neuropathy before starting GLP1RA treament.
Other causes of gastroparesis include:
- some viral infections (eg Norwalk, rotavirus)
- medications that slow the stomach (eg narcotics, calcium channel blockers (used for hypertension or to slow heart rate), tricyclic antidepressants, and many others)
- previous thoracic (chest) or gastric (stomach) surgery causing damage to the vagus nerve (which innervates the stomach)
- neurologic disorders (eg multiple sclerosis, Parkinson’s disease)
Some news outlets have suggested that stomachs can become permanently ‘paralyzed’ by GLP1RAs after stopping medication due to GI intolerance. To my knowledge, there is no evidence to support permanent/irreversible gastroparesis brought on by GLP1RAs in the medical literature, though we must always take any new case reports or information seriously, when presented and discussed by medical professionals (not by news media).
BOTTOM LINE: GLP1 receptor agonists slow gastrointestinal transit. If gastrointestinal symptoms occur, these are mild to moderate and transient in most cases. Having gastrointestinal side effects does not mean that a person has a diagnosis of gastroparesis. People with slowing of gastrointestinal transit prior to starting GLP1RAs may be at higher risk of GI side effects. GLP1RAs are not known to cause permanent gastroparesis after stopping medication. As always, we remain vigilant of any new medically peer-reviewed cases, data or evidence as for any medication.
Note: This blog is not a substitute for personal medical advice. Discuss any concerns you may have with your health care provider.
PS A special shout-out to my colleague Dr Akshay Jain who gave a great webinar on the topic of gastroparesis earlier this year, for health care professionals – check it out here!
Disclaimer: I am/have been an investigator in clinical trials of liraglutide and semaglutide. I receive honoraria as a continuing medical education speaker and consultant from the makers of liraglutide and semaglutide (Novo Nordisk) and exenatide (Astra Zeneca).
Share this blog post using your favorite social media link below!
Follow me on twitter! @drsuepedersen
www.drsue.ca © 2023