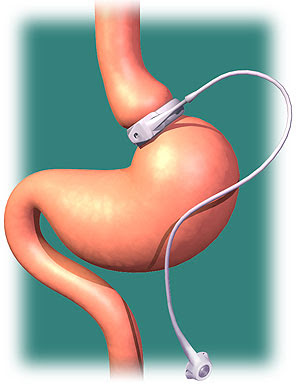
As for any medical treatment or surgery, the decision to undergo bariatric surgery requires that the benefits and risks are carefully evaluated by the patient and the health care team. Amongst the list of benefits, several studies have suggested that bariatric surgery decreases the risk of cancer amongst women. Now, a new study suggests that the risk of colorectal cancer may actually be increased after obesity surgery.
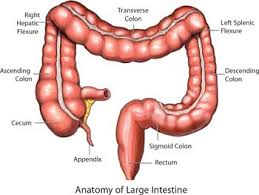
The study was an evaluation of the population database in Sweden, looking at the colon cancer incidence rates amongst men and women who had obesity surgery (gastric bypass, gastric banding, and an older procedure called vertical banded gastroplasty), compared to patients with obesity who did not have bariatric surgery. They found that amongst those who had had bariatric surgery, the risk of colon cancer was 60% higher than those who hadn’t had surgery (though the absolute numbers were fairly low – 70 out of 15,095 patients, or 0.46% of patients who had obesity surgery developed colon cancer). Ten years after bariatric surgery, the risk of having colon cancer was double compared to people with obesity who hadn’t had bariatric surgery.
These results need to be taken with a grain of salt, as there are a number of limitations to this database analysis – for example, other risk factors associated with colon cancer such as smoking, diabetes, family history etc were not available (the interested reader can read more about this here). The study does seem to contradict the overall protective effect that bariatric surgery is thought to have on cancer risk (for women, at least) – but then again, most previous studies have not followed up patients for as long as this one, and colon cancer is known to be a very slow growing tumor.
Following gastric bypass surgery, it has been suggested that the lining of the intestine may change (called ‘mucosal hyperproliferation’), and an increase in a pro-tumor chemical has been found (a cytokine called ‘macrophage migration inhibitory factor’), though other tumor inducing chemicals (such as TNF alpha and interleukin 6) have been shown to decrease after bariatric surgery. The population of intestinal bacteria change after surgery as well, and there is still much we don’t know about the effects of these changes (though there appear to be metabolic benefits of these post-surgery bacterial changes).
So where does this leave us? Well, there are still many questions to be answered about the long term efffects of bariatric surgery, which only time will teach us. In the meantime, we must continue to carefully weigh the benefits and risks of obesity surgery, and for patients who have had bariatric surgery, colon cancer screening and surveillance should be undertaken.