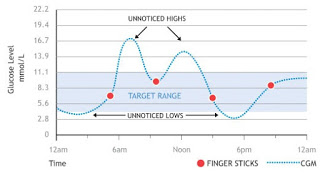
In people with diabetes, continuous glucose monitoring (CGM) is an alternative to checking sugars with frequent finger pokes. CGM is available as a stand alone tool, or can be integrated with an insulin pump system. Most studies showing the benefits of CGM were done in people using insulin pumps. Now, two studies show the benefits of CGM in people with type 1 diabetes using insulin injections to treat their diabetes.
The first study, published in JAMA, randomized 158 people with type 1 diabetes using insulin injections to use of either the usual form of self blood glucose monitoring (finger pokes) vs CGM. At 6 months, the hemoglobin A1C (a marker of diabetes control) was 0.6% lower in the people using CGM compared to those using finger pokes. People using finger pokes to check sugars during the study were also wearing a CGM during the study, but they could not access the readings on the CGM, with the purpose being for researchers to analyze what the CGM showed in the people using finger pokes during the study. Importantly, this analysis found that people using CGM spent 37 minutes less per day with low blood sugar (43 minutes per day, compared to 80 minutes per day for people using finger pokes).
The second study, also published in JAMA, compared the effect of CGM vs finger poke monitoring in the same person, using a crossover design. Patients were randomized to use either CGM or finger pokes for 6 months, then did the reverse for the next 6 months (with a 17 week break in between). Amongst these 161 patients with type 1 diabetes, hemoglobin A1C was 0.43% lower during the time of CGM use, and they also reported less fear of hypoglycemia, greater well being and greater treatment satisfaction while using CGM. Patients were hypoglycemic 4.79% of the time while using finger pokes (using data from masked CGMs), vs 2.79% of the time with use of CGM.
One thing that I found particularly disturbing about these studies was the amount of time patients spent with low blood sugars. While CGM improves upon this, we would ideally like patients with diabetes to have zero hypoglycemia. CGM units have alarms that alert a patient when blood sugar is low, which can be lifesaving, especially for people who don’t feel their low sugars and are at risk of sleeping through a low. Hopefully improved glucose monitoring technology, as well as better insulins being developed, will help us to reduce lows further. CGMs are unfortunately quite expensive, though some people are able to get the expense covered – talk to your insurance provider (if you have one) and/or your diabetes educator to find out about your options.
These studies clearly support the potential benefits of continuous glucose monitor (CGM) use in people with type 1 diabetes using insulin injections.