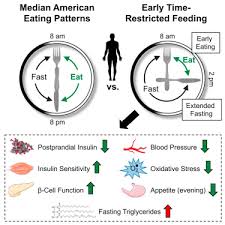
In the quest to find treatment strategies for COVID-19 infection, one class of medications that have been considered is the SGLT2 inhibitors. These are medications used to treat type 2 diabetes, heart failure, and provide excellent kidney protection for people with chronic kidney disease (see previous blogs here and here and here and here). The thinking is that mechanisms by which the SGLT2 inhibitors protect the heart and kidneys in people with and without type 2 diabetes overlap substantially with those triggered in a COVID-19 infection, including improving extracellular fluid overload and reducing inflammation.
The DARE-19 trial randomized 1,250 adults hospitalized with COVID-19 and at least one risk factor for COVID-19 complications (hypertension , type 2 diabetes, heart failure, chronic kidney disease, and/or atherosclerotic cardiovascular disease), and randomly assigned them to dapagliflozin (Forxiga) 10mg vs placebo for 30 days. The goal was to see if dapagliflozin could reduce new or worsened organ dysfunction or death, or hasten recovery. About half of patients in this study had type 2 diabetes, with about two thirds of those being on insulin at baseline. Seven countries participated (USA, Canada, Mexico, Brazil, Argentina, India, and UK). Over the course of the study, 11% of patients in each group were discontinued from study medication.
At 30 days, organ failure or death occurred in 11.2% of people in the dapagliflozin group vs 13.8% of the placebo group, which was numerically lower in the dapagliflozin group, but not a statistically significant difference. There was also no significant difference in death between groups (6.6% in the dapagliflozin group vs 8.6% in the placebo group). Time to recovery (hospital discharge) was similar between groups. At the recent American Diabetes Association meeting, researchers demonstrated that these findings were consistent among those with and without type 2 diabetes.
The investigators note that COVID is changing, and this study was started quite early in the pandemic (April 2020). It would be interesting to know if these results would become statistically significant in a larger study, or whether the results would look any different with the current 2021 standards of care for COVID.
For people who are on dapagliflozin or any other SGLT2 inhibitor [canagliflozin (Invokana) or empagliflozin (Jardiance)], we advise stopping these medications if they are sick and unable to hydrate normally (including when admitted to hospital). This is because SGLT2 inhibitors increase urination and can lead to dehydration (which could lead to acute kidney damage), and also due to an increased risk of diabetic ketoacidosis (DKA) in people with diabetes. In this study, there were actually numerically lower acute kidney events in the dapagliflozin group (21, vs 34 in placebo). There were 2 episodes of DKA in the dapagliflozin group, vs none in placebo. Thus, the DARE-19 study suggests that dapagliflozin was not only well tolerated in hospitalized patients, but hints at the possibility of organ protection. As a medical community, with these and other emerging data, we should reconsider whether all patients on SGLT2 inhibitors admitted to hospital should have this medication stopped, or whether it may actually be appropriate to cautiously continue (or even start new) for the health benefits they provide.
Disclaimer: I receive honoraria as a continuing medical education speaker and consultant from the makers of dapagliflozin (Astra Zeneca), empagliflozin (Boehringer Ingelheim/Eli Lilly), and canagliflozin (Janssen). I have been involved as an investigator in clinical trials of SGLT2 inhibitors.
Share this blog post using your favorite social media link below!
Follow me on twitter! @drsuepedersen
www.drsue.ca © 2021