Ninety percent of people with type 2 diabetes carry elevated body weight. The metabolic abnormalities that ultimately lead to type 2 diabetes begin many years before diabetes actually develops, with weight gain and central obesity leading to progressive insulin resistance. Despite this close interconnection between type 2 diabetes and elevated body weight, the current diabetes treatment framework and guidelines are primarily focused on treating the ‘downstream’ metabolic consequences of carrying elevated body weight years later (blood sugars, cardiovascular protection).
While it is extremely important to treat blood sugars and prevent/treat the longer term heart/kidney complications of diabetes, what if we shift our focus on treatment early in diabetes towards weight management?
In a recent paper, published in The Lancet, Lingvay and colleagues propose an ‘upstream’ approach, targeting weight management early on in diabetes, as opposed to our current ‘downstream’ approach, which focus on blood sugar control and prevention/management of complications that arise later on.
Let’s first consider prediabetes – when sugars are not normal, but have not yet risen into the diabetes range. If we focus on weight management at this stage, we can help keep the pancreas healthy, reduce insulin resistance, and prevent diabetes from developing. Amongst people with prediabetes, losing just 1kg (2.2lb) of weight reduces the risk of developing diabetes by 16% (more on these data here).
Weight management medications are an important tool in our upstream approach. Several weight management medications have been shown to help put prediabetes into remission and prevent development of type 2 diabetes. With new and emerging obesity medications, we are now seeing well into double-digit weight loss, which has important implications for not only blood sugars, but a long list of other metabolic and mechanical complications of obesity, and importantly, a better quality of life.
Let’s now move on to a person who is fairly early on in their diabetes journey. At this point, because insulin resistance and weight have progressed, and the pancreas is more fatigued, remission of type 2 diabetes requires more weight loss than remission of prediabetes . The available data suggests that 10-15% weight loss is required to induce diabetes remission. This degree of weight loss is difficult for most people to achieve, and even harder to sustain, without the help of treatment strategies beyond lifestyle changes – this is the natural biology of obesity at work. Once diabetes develops, it is also harder to lose weight (more on why here).
In the treatment of type 2 diabetes, two classes of diabetes medication provide important heart and kidney protection (GLP1 receptor agonists and SGLT2 inhibitors), facilitate weight loss, and don’t cause low blood sugars. Thus, prioritizing GLP1 receptor agonists and SGLT2 inhibitors fit the bill of providing cardiovascular and kidney protection, controlling blood sugars, and helping with weight loss. Emerging medications for type 2 diabetes also hold promise for double-digit weight loss.
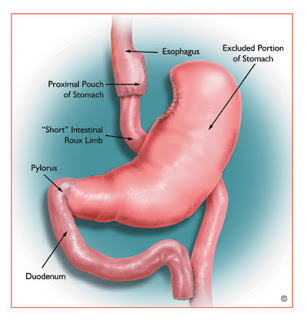
Bariatric surgery is an effective treatment for obesity in people with type 2 diabetes, with many people enjoying diabetes remission after surgery. Again here, intervening further upstream (earlier in the diabetes journey) is beneficial, as predictors of diabetes remission include younger age, shorter duration of diabetes, and higher preoperative C-peptide levels (an indicator of the pancreas’ ability to produce insulin).
The authors contend that the initial treatment goal in people with type 2 diabetes and obesity should be to achieve and maintain 15% weight loss, to achieve best chance of diabetes remission, and to reduce cardiovascular risk. This is very hard to achieve with lifestyle change alone, but thankfully, there are new and emerging medications, and/or bariatric surgery for the appropriate patient, that can help with this. This goal is now becoming accessible with the advent of these treatment options.
In parallel to weight management, we must also address glucose lowering, and cardiorenal protection, as we do now. But if we focus on weight management early on, we can help to prevent more difficult to control glucose and cardiovascular/kidney complications later on, for many people.
BOTTOM LINE: As the authors write,
It is time to consider shifting the treatment focus for patients with type 2 diabetes from the current reactive glucocentric (sugar lowering) approach to addressing obesity, the core driver of insulin resistance and contributor to B-cell failure (tired pancreas). Management of obesity is not a competitor, but an addition to existing treatment goals. Strategies that result in substantial and durable weight loss can disrupt the disease course of type 2 diabetes.
Share this blog post using your favorite social media link below!
Follow me on twitter! @drsuepedersen
www.drsue.ca © 2022