While it is well known that about 90% of people with type 2 diabetes have elevated body weight, it is often overlooked that many people with autoimmune type 1 diabetes also struggle with elevated weight (as do the majority of adults in most developed countries).
At the 2022 Diabetes Canada/Canadian Society of Endocrinology & Metabolism (DC/CSEM) conference today, I was asked by conference organizers to give a talk in which to specifically address the question: Can obesity medication be part of the weight management strategy in people with type 1 diabetes and obesity?
While today’s blog post is specifically about obesity medications in type 1 diabetes, I first want to point out that it’s important to consider specific drivers of weight gain in people with type 1 diabetes. Specific challenges can include:
- Non physiological insulin replacement (ie, insulin treatment does not perfectly match what the normal functioning pancreas would produce)
- Administering insulin under the skin, instead of having it produced directly by the pancreas, bypasses the effects of insulin on the liver and may result in higher insulin levels and fat accumulation
- Defensive/extra snacking to avoid hypoglycemia (low sugar)
- Disordered eating (eg due to intense emphasis placed on food/carb intake, depression, or other factors; this may be especially common among younger women)
- Fear of hypoglycemia can be a deterrent from being active
It is of critical importance to address any of the above issues, as well as potential causes/contributors to elevated weight that can be present in anyone with elevated weight, in helping a person with type 1 diabetes manage elevated weight.
Weight gain can have a negative impact on compliance with insulin treatment and blood sugar control. Some people may be tempted to underdose their insulin to achieve weight loss, which comes at the consequence of higher sugars, a higher risk of diabetic ketoacidosis (DKA) which can be life threatening, and a higher risk of complications over time.
Unfortunately, obesity medications haven’t yet been studied in people with type 1 diabetes. Liraglutide, which is approved at a dose of 1.2mg or 1.8mg daily (Victoza) for type 2 diabetes, and at 3mg daily (Saxenda) for weight management in people with or without type 2 diabetes, has been studied at the diabetes treatment dosing in people with type 1 diabetes in the ADJUNCT One and ADJUNCT Two trials. (I was one of the investigators in the latter study). In these trials, liraglutide was studied at 0.6mg, 1.2mg, and 1.8mg vs placebo for 26-52 weeks in over 2,000 participants with type 1 diabetes. These studies found a dose dependent weight reduction of approximately 2.5 to 5 kg (baseline weight 84-86kg, baseline BMI approximately 29), a reduction in A1C ranging from 0.2-0.5% (baseline 8-8.1%), and improvement in quality of life. There was more symptomatic hypoglycemia (low blood sugar) likely due to too little insulin reduction in those patients, and more hyperglycemia (elevated blood sugar) with ketosis, likely due to too much insulin reduction in those patients.
As for the other three obesity medications approved in Canada (semaglutide 2.4mg (Wegovy)), naltrexone/bupropion (Contrave), and orlistat (Xenical), there are no studies in type 1 diabetes. Semaglutide is available as a treatment of type 2 diabetes (called Ozempic) at a dose of 0.5mg, 1mg, or 2mg weekly, but has not been studied in people with type 1 diabetes.
If a health care provider were to consider prescribing a weight loss medication (off label) to a person with type 1 diabetes, considerations include:
- reduction in insulin where needed to avoid low blood sugars, with starting or escalating a GLP1RA (liraglutide or semaglutide)
- reduction in mealtime insulin for any medication that decreases appetite (liraglutide, semaglutide, naltrexone/bupropion)
- reduction in insulin as needed with weight loss, for avoidance of low blood sugar (any obesity medication)
- considering and managing gastrointestinal side effects, particularly nausea, which can affect food intake and insulin needs (liraglutide, semaglutide, and naltrexone/bupropion, can all have nausea as a side effect)
BOTTOM LINE: Obesity is an important health issue, including amongst people with type 1 diabetes. We lack data on the use of obesity medication in people with type 1 diabetes, and studies are urgently needed!
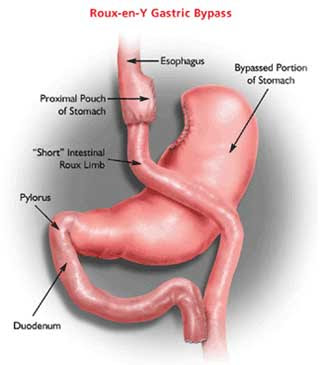
For more reading on the similar paucity of data for weight management with lifestyle changes and bariatric surgery in type 1 diabetes, check out this excellent recent review article, published in Lancet Diabetes & Endocrinology.
Disclaimer: I am an investigator and coauthor of several studies of liraglutide and semaglutide. I receive honoraria as a continuing medical education speaker and consultant from the maker of liraglutide and semaglutide (Novo Nordisk), and naltrexone/bupropion (Bausch).
Check me out on twitter! @drsuepedersen
Share this blog post using your favorite social media link below!
www.drsue.ca © 2022