After years – decades – of available weight loss medications falling short of desired weight loss, it is perhaps something of a luxury that the concept of ‘too much’ weight loss has become a possibility that needs to be discussed. This topic was recently addressed in a round table review published in Obesity Pillars , the official publication of the Obesity Medicine Association in USA.
What is too much weight loss? Excessive weight loss could be defined as:
- The person (patient) being uncomfortable or unhappy with their weight being too low
- Excessive depletion of muscle mass (sarcopenia)
- A person feeling unwell or weak due to excessive weight loss
- A BMI of <18.5 (for most people)
Things for the health care provider to consider in a patient with excessive weight loss:
- Consider whether your patient needs investigation for other possible causes of weight loss. Are there any red flags to suggest something else is going on?
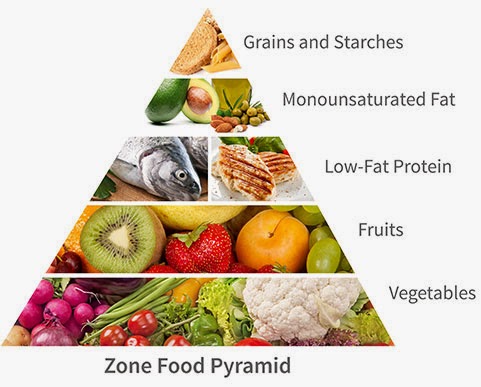
- Is your patient getting adequate nutritional intake and protein intake?
- In some cases, a complaint of excessive weight loss may actually reflect a person feeling uncomfortable with their new body image, shape and/or size. Or, there could be a concern about a change in relationships or lifestyles that make it harder to engage with their usual social or cultural activities. Psychological support can be beneficial in these situations.
- If a family member is the person with concerns, this can certainly be well founded, but can also sometimes be without the person’s health in mind. Some people can feel insecure, jealous, or resentful if their partner/family member/friend is losing weight. The person’s family or friends may be feeling left out of the patient’s new lifestyle habits or routines.
- Be sure to ask about side effects of obesity medications. Some people may be accepting excessive gastrointestinal side effects (causing excessive weight loss) because they so desperately want to lose as much weight as possible.
- Weight loss may improve depression or anxiety, but in some cases, these could actually worsen, for a multitide of potential reasons. Some people eat less when they feel depressed or anxious. Evaluating the relationship between mental health and eating patterns/behaviours is important throughout the weight management journey, as it can also change with weight change.
- Discuss physical activity, and how/whether it has changed with weight loss. Increasing physical activity can help to maintain muscle mass, and many people feel more able to become more active after losing a substantial amount of weight. If a person is feeling weak and/or unable to increase physical activity, this can be a sign that weight loss is excessive (or that some other health issue is presenting itself, as per the first point above).
While the round table review article suggests that highly effective obesity medications may not be the best first choice in people with pre-obesity (which I believe they are defining by lower BMI criteria, likely BMI 25-30 or 27-30) or class 1 obesity (BMI 30-35), I don’t necessarily agree with this advice. While one of the less powerful obesity medications could certainly be utilized in people with a milder elevation in BMI, it is also entirely reasonable (in my opinion) to choose one of the more powerful obesity medications, but to use a lower dose. We need to start thinking about obesity medications as titratable treatments. One dose does not fit all.
An analogy I like to draw here is to insulin use in treatment of type 2 diabetes. Some people need 10 units of insulin per day, while others need several hundred units per day. Thus, we start at a low dose, and titrate to the desired effect of controlled blood sugars. We would never dream of prescribing everyone the same insulin dose. For some people it wouldn’t be enough; for others, that same dose could cause life threatening low blood sugar.
Similarly, with obesity medications, a lower dose may be all that one person needs to achieve treatment targets (which can include any/all of improvement in metabolic health, mechanical health, mental health, weight loss, and quality of life). Others may need the maximum dose to reach or get closer to treatment goals. Some may not tolerate the full dose, or are not able to afford more than a certain dose financially, so they take what their body (or pocketbook) can tolerate. For some people with excessive weight loss with obesity medication, all that may be needed (after assessing points above) is to dial the dose down, reassess, and partner with your patient to determine what dose is best for them.
Share this blog post using your favorite social media link below!
Check me out on twitter! @drsuepedersen
www.drsue.ca © 2022