Lipedema is a medical condition that often goes overlooked, often being put into the same diagnostic category as obesity. Lipedema, however, is not only distinct from obesity, but also much more common that previously thought. As such, a standard of care for lipedema in USA is available to guide health care providers and patients on recognizing and treating this serious medical issue.
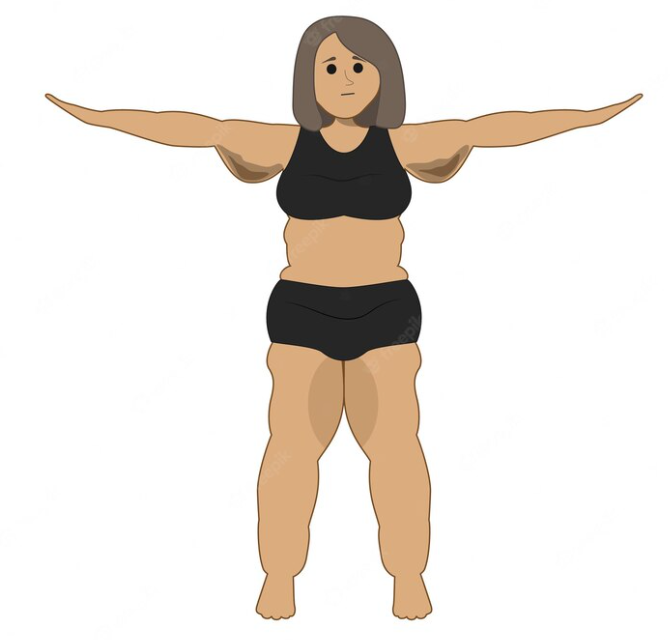
Lipedema is an inflammatory condition seen predominantly in women, where painful, nodular, fibrotic (scarring) fat tissue develops on buttocks, hips, lower abdomen, and limbs. It often begins at times of hormone, weight, and/or shape change, such as puberty, childbearing, menopause, stress associated with lifestyle change, or by altering tissue structure after surgery or trauma. People with lipedema are often stigmatized by health care professionals as well as general society; both the disease and its associated stigma can have a profoundly negative impact on quality of life.
Lipedema is now recognized to be much more common that previously thought, affecting an estimated 6-8% of women in a German study, and 15-19% attending vascular clinics. It often runs in families. Due to the increased leg size seen with lipedema, this condition is often confused with obesity or lymphedema (swelling due to lymphatic drainage issues).
Key features that point to lipedema include:
- tissue nodules are palpable (can be felt)
- tissue is often painful (though not always)
- hands and feet are not affected – look for a tissue ‘cuff’ at the ankle or wrist where the abnormal fat tissue stops (though some can have fat tissue on eg hands, it is not painful nodular tissue)
- legs continue to appear swollen despite elevation (whereas edema due to lymphatic drainage issues tends to decrease with leg elevation)
People with lipedema can also have obesity, and can also have lymphedema.
It is also important to evaluate the arterial and venous systems in people with lipedema. Peripheral arterial disease (narrowing of the arteries due to atherosclerotic disease) can be missed if leg pain is ascribed to lipedema without thinking about this possibility. People with lipedema are also at higher risk for blood clots in the legs, called deep venous thrombosis (DVT), which can lead to potentially life threatening pulmonary embolism (PE). People with lipedema are also at higher risk of other conditions associated with chronic venous disease.
Unfortunately, treatment approaches are currently very limited. Manual therapies (eg soft tissue mobilization) and compression garments/pumps can decrease pain, stimulate lymphatic flow and reduce edema (swelling).
While recommended, lipedema doesn’t tend to improve much with lifestyle approaches (though responses differ from person to person). One non-randomized study suggested that a low carb high fat diet may be beneficial, and a possible benefit of the keto diet has been hypothesized, with reduction in inflammation postulated as one of the mechanisms of benefit. (read more about definitions and challenges of low carb diets here, and keto diet here).
Existing knowledge suggests that bariatric surgery also has limited success in treating lipedema, likely due to the fibrotic (scarring) component of the connective tissue.
Lipedema reduction surgery (including liposuction) can be very beneficial, improving symptoms, mobility, and quality of life, but access is unfortunately extremely limited.
Another area where there is a gap in knowledge, is whether new or emerging obesity medication can help to treat lipedema. As inflammation is a hallmark of lipedema, strategies that reduce inflammation could benefit lipedema. Weight loss itself can reduce inflammation; the GLP1 and GIP/GLP1 receptor agonists in particular have been suggested to have an anti-inflammatory mechanism of action, in addition to facilitating weight loss (see here and here).
BOTTOM LINE: Lipedema is common, often missed, often painful, and can profoundly impair quality of life. Further studies to find effective treatment approaches, and access to these treatments, are desperately needed.
Check me out on twitter! @drsuepedersen
Share this blog post using your favorite social media link below!
www.drsue.ca © 2023