My recent blog post on this question – Does obesity go into remission? – has generated a lot of interest and great conversation.
I have had colleagues and patients share stories with me, mostly reflecting on how hard they (or their patients) need to work in order to maintain successful weight loss and continued improvements in their health. This message has been especially strong from those who have managed to lose weight and keep it off with lifestyle changes alone (more on the physiology behind this here). I’ve had people who have had bariatric surgery tell me that while surgery allowed them to feel the sense of fullness for the first time, they still need to manage the hunger that they feel at their new lower weight, with daily attention to lifestyle choices. People who have tried stopping weight loss medication (remember, you have to be on no treatment to be considered in ‘remission’) tell me almost uniformly that their appetite drives come back with a vengeance and weight starts going back up.
On the other hand, I’ve also had a few people share that they do feel, following a permanent lifestyle change, that their obesity is in remission. While they do reflect that they still need to be attentive, they don’t feel an intense hunger, and feel able to maintain their lower weight without too much trouble. The drive for weight regain is perhaps not as biologically powerful for these individuals. (I would also emphasize that it is very much the exception, not the rule, to feel this way). I’ve had some people who have had bariatric surgery share that they feel a good hunger/fullness balance at their lower weight, and are likewise able to maintain without too much trouble. These people most likely have more powerful hormonal changes after bariatric surgery that are helping them to have this more manageable hunger/fullness balance. (again, this is the exception – more on the typical increase in hunger and decrease in satiety after weight loss from bariatric surgery in this excellent article)
In thinking about situations where obesity perhaps could go into remission, another situation to consider is what happens when people who have gained weight and weight-related health complications due to a medication (eg steroid treatment, like prednisone), stop that medication. Many people retain the weight that has been gained, but some people do seem to readily shed that weight.
So why does the occassional person feel like they don’t have to work ‘that hard’ to keep weight off? And why do many people retain weight after a health event that causes weight gain (eg medications or pregnancy), but others shed the pounds with relative ease?
The influencing factors here are many, diverse, and complex, but two key determinants are likely inflammation and genetics.
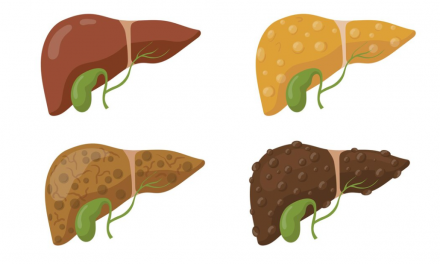
We know that obesity is a state of low-grade inflammation, and that inflammation causes damage and scarring to the appetite center in our brain (hypothalamus) over time. This causes the appetite center to dysfunction, causing the ‘set point’ of hunger and fullness to be reset to the higher body weight. If obesity has only been present short term, there may not be enough time for the inflammatory state to cause damage, so the body more readily sheds the weight (and keeps it off) when the weight-increasing stimulus is no longer present.
As for genetics – as blogged previously, genetics have a powerful role in determining not only where our body weight ‘wants’ to be, but also strongly influences our body shape and body composition. Genetics influence every aspect of weight balance, from our body’s hunger/fullness hormone balance and response, to the inflammatory response, to a long list of other parameters and factors.
A special thanks to my Canadian obesity physician colleagues who had a lot of great input and feedback on this topic!
Let’s keep this conversation going!
Check me out on twitter! @drsuepedersen
Share this blog post using your favorite social media link below!
www.drsue.ca © 2023