Prefer to listen? Check out my podcast here!
In follow up to my blog post a few days ago, the DiRECT trial 5 year results have now been published, and the global diabetes and obesity communities are in heated debate about its implications.
The DiRECT study was a 2 year randomized controlled trial, assessing the efficacy of an intensive lifestyle program to induce remission of type 2 diabetes. The 5 year obeservational extension results were published in The Lancet Diabetes & Endocrinology. (coincidentally, within hours of my blog post about whether diabetes remission with lifestyle change is a realistic long term goal).
The DiRECT study enrolled 298 adults in the UK with type 2 diabetes diagnosed for 6 years or less, BMI 27-45 kg/m2, and not receiving insulin. They were placed on a total diet replacement formula providing about 850 calories per day for 12 weeks, followed by stepped food reintroduction over 6-8 weeks, then structured support for weight loss maintenance. A nurse or dietitian supported patients with 30 minute appointments every 2 weeks until food reintroduction was completed, and then monthly for maintenance. After the 2 year randomized trial was complete, 94 intervention participants continued into the 3 year extension, with continued support with 15-30 minute appointments every 3 months.
The 5-year results paper contains a whole lot of calculations on remission rates, with various denominators. I am not going to dissect these numbers in today’s post. The bottom line is this: while 46% of people in the intervention group (68 out of 149) were in diabetes remission at one year, only 7% of the original intervention group (11 out of 149) were in diabetes remission at the 5 year mark. The return of diabetes coincides with weight regain: while 61 people in the intervention group had lost at least 10kg at the 1 year mark, only 21 people (14%) in the original intervention group were still at least 10kg below their baseline weight at 5 years. We must also remember that weight was self reported, and people tend to under report their weight. When reviewing the results of this study, it’s also important to note that the people who participated in the 5 year extension were self-selected, in that only those who remained engaged with the intervention at 2 years were offered enrolment in the extension study.
The authors comment that the DiRECT 5 year program was designed to help patients achieve and stay in diabetes remission, entirely within routine primary care. While their protocol of visits every 3 months for years 3-5 may be feasible for some practices, I would not agree that their meal replacement protocol and first 2 years of highly frequent visits is something that most primary care practices can accomodate.
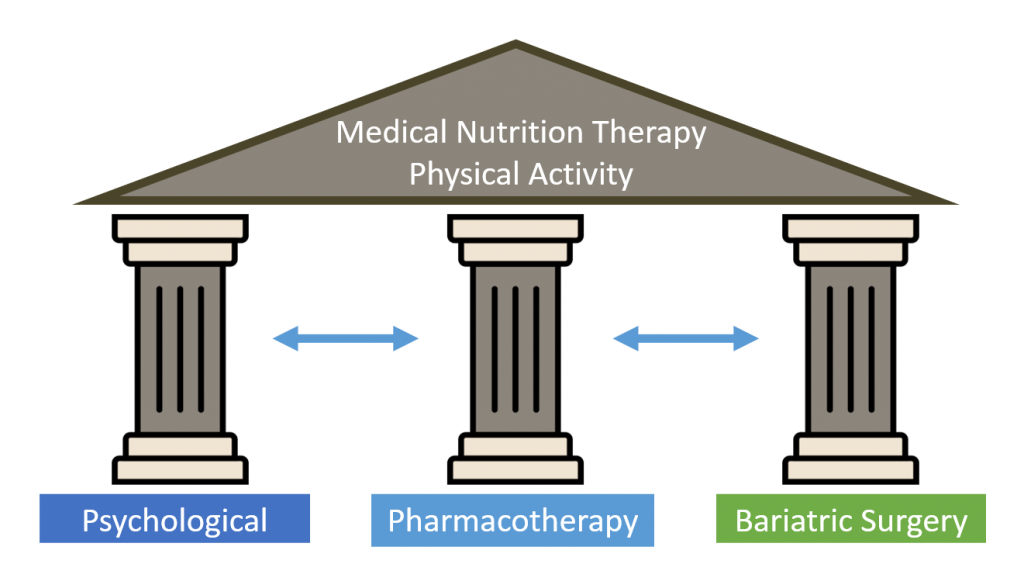
Again, at the end of the day, I am underwhelmed by the DiRECT trial results. The lifestyle intervention is not feasible for most clinics to support. While any time in diabetes remission is good for health (as previously blogged), very few are in remission long term. The central issue here, that isn’t discussed much in the paper, is that obesity is a chronic medical condition that goes hand in hand with type 2 diabetes (in most cases). It defies natural human biology to advise people to just ‘keep on keeping on’ with lifestyle changes (more on this here and here). As per our Canadian Obesity Guidelines, diet and exercise are not treatments for obesity in and of themselves. The Three Pillars of Weight Management (psychological support, medications, and/or bariatric surgery) help people to stick with healthier lifestyles. Think of it this way: if you don’t have any pillars to support the roof, the roof is most likely to cave in.
In my opinion, we would be remiss as health care providers to encourage people with type 2 diabetes down the path of a lifestyle program alone, as this is unlikely to be met with long term sustained improvements in health, may set people up for a sense of failure, and does not take into account the holistic overall needs and care of people also living with obesity. Not to mention that there are important medications for diabetes that provide important protection of the heart and kidneys, and can help people in their weight loss efforts. I will never ‘direct’ my patients, but I will continue to support them in a holistic way to advise them on the options, the data, and the science, and partner with each person to choose a care path that is best for them.
Check me out on X/twitter! @drsuepedersen
Share this blog post using your favorite social media link below!
www.drsue.ca © 2024