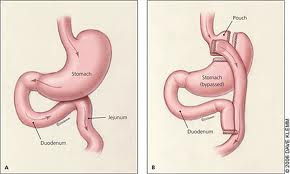
Bariatric surgery is one of the treatment options for people with severe obesity, and often, patients having surgery are women of reproductive age. We know also that bariatric surgery can often improve fertility. While lower weight before pregnancy can decrease many health risks to both mum and baby, there are also risks to pregnancies after bariatric surgery, including having a small for gestational age baby, preterm birth, and congenital anomalies. So how do we best support and care for women after bariatric surgery, to help them plan and progress through the most successful pregnancy possible?
A set of consensus recommendations on this topic was recently published in Obesity Reviews by Shawe and colleagues. Here are some of their key points:
- Contraception (to avoid an unplanned pregnancy) is essential.
Avoid oral contraceptives as they may be less effective, and are also associated with an increased risk of blood clots. An IUD (intrauterine device) may be the best choice for most women. A contraceptive diaphragm may be difficult to insert correctly and requires refitting after every 3kg of weight change. - How long after bariatric surgery should you wait to get pregnant?
Postpone pregnancy until weight has stabilized (1-2 years). (some studies suggest longer is better) - Dietary issues in pregnancy: it’s important to eat right for the pregnancy, as well as meet the body’s special needs after having had bariatric surgery. Aim for at least 60g of protein per day. Special attention may need to be given to carbohydrate quantity and quality, particularly in those who have high sugars, low sugars, or trouble with dumping. (see the paper for more details)
- It is essential to take the appropriate nutritional supplements (vitamins) before and during pregnancy – these atually need to be optimized 3-6 months before trying to get pregnant.
- Nutrient levels to check before and during pregnancy (and how often) – ensuring levels are at targets before trying to get pregnant, and during pregnancy, as needs for many vitamins and minerals can increase in pregnancy.
- Screening for diabetes: women with obesity are at a higher risk of having diabetes both before pregnancy, as well as developing it during pregnancy, though this risk is lowered after bariatric surgery. One of the tests used to screen for diabetes is the oral glucose tolerance test (OGTT), which can cause dumping or hypoglycemia after bariatric surgery, and this test may also not be as accurate after bariatric surgery. Instead, they suggest checking sugars 7 times per day, or using a continuous glucose monitor, in place of where OGTT would otherwise have been recommended.
- Weight management in pregnancy: most people struggle with weight regain after bariatric surgery. Thus, we want to avoid excessive weight gain in pregnancy, but we need to ensure that mom is gaining enough weight in pregnancy to ensure babe is growing well. They recommend following standard recommendations for weight gain in pregnancy based on body mass index (BMI) pre pregnancy, but with the caveat that surveillance of babe is paramount to ensure baby is growing well.
- Fetal monitoring – for size (as there’s a higher risk of fetal growth restriction and being small for gestational age), and also for congenital abnormalities, as this risk is higher if there are any nutritional deficiencies.
- Breast feeding – yes it’s recommended! The composition of breast mild from women after bariatric surgery is largely comparable to women who haven’t had surgery. Importantly, mom’s nutritional parameters need to be monitored closely (blood tests).
They also discuss assessment and prevention of surgical complications in pregnancy, and the importance of addressing mental health issues in pregnancy.
Dr Sue Pedersen www.drsue.ca © 2019
Follow me on Twitter! @drsuepedersen